-
肌间沟臂丛阻滞(interscalene brachial plexus block, ISB)是肩关节镜手术的常用麻醉方式[1],但膈神经麻痹(hemidiaphragmatic paresis,HDP)的发生率高,对术前合并呼吸系统疾病的患者不利[2]。此外,肌间沟臂丛阻滞还会导致术后长时间的上肢感觉及运动障碍,降低患者满意度及舒适度[3]。Kim等[4]与Kang等[5]于近期报道臂丛上干阻滞(superior trunk block,ST)应用于肩关节镜手术可以有效减少HDP的发生,同时对肌力的影响更小。周阳洋等[6]报道低浓度低剂量(0.375% 10 ml)罗哌卡因行臂丛上干阻滞,完全的HDP发生率为0,还能提供良好的术后镇痛,保留患肢部分肌力,提高患者舒适度,但部分HDP发生率较高(87.2%)。为进一步探究降低部分HDP发生率的可能性,本研究采用更低浓度(0.25%)的罗哌卡因比较肌间沟与臂丛上干阻滞用于肩关节镜手术的临床效果。
-
本研究获得海军军医大学第二附属医院伦理委员会批准(CZEC2020-10),所有患者及家属均签署知情同意书。选择2020年8月至12月于本院择期行肩关节镜下肩袖修补术的患者46例,男22例,女24例,年龄26~70岁,BMI (24.5±2.5)kg/m2,ASA I~Ⅱ级。排除标准:①神经阻滞禁忌证;②长期服用镇痛药物;③不能理解疼痛评分;④不能配合完成握力检查及膈肌移动度检查。采用随机数字法(n=46)分成2组:超声引导下肌间沟臂丛神经阻滞组(ISB组)和臂丛上干阻滞组(ST组)。
-
患者入室后监测心电图、脉氧饱和度,桡动脉穿刺监测有创动脉压。
-
ISB 组与ST组所用的药液均配制成浓度为 0.25% 10 ml罗哌卡因。取5 ml 0.75%罗哌卡因,加入0.9%氯化钠注射液10 ml,配制成浓度为0.25%的15 ml溶液,取10 ml 备用。
-
取用 2 ml 盐酸右美托咪定注射液(规格 2 ml:200 µg)加入 48 ml 0.9% 氯化钠注射液,配制成50 ml 浓度为 4 µg/ml 的 总溶液。
-
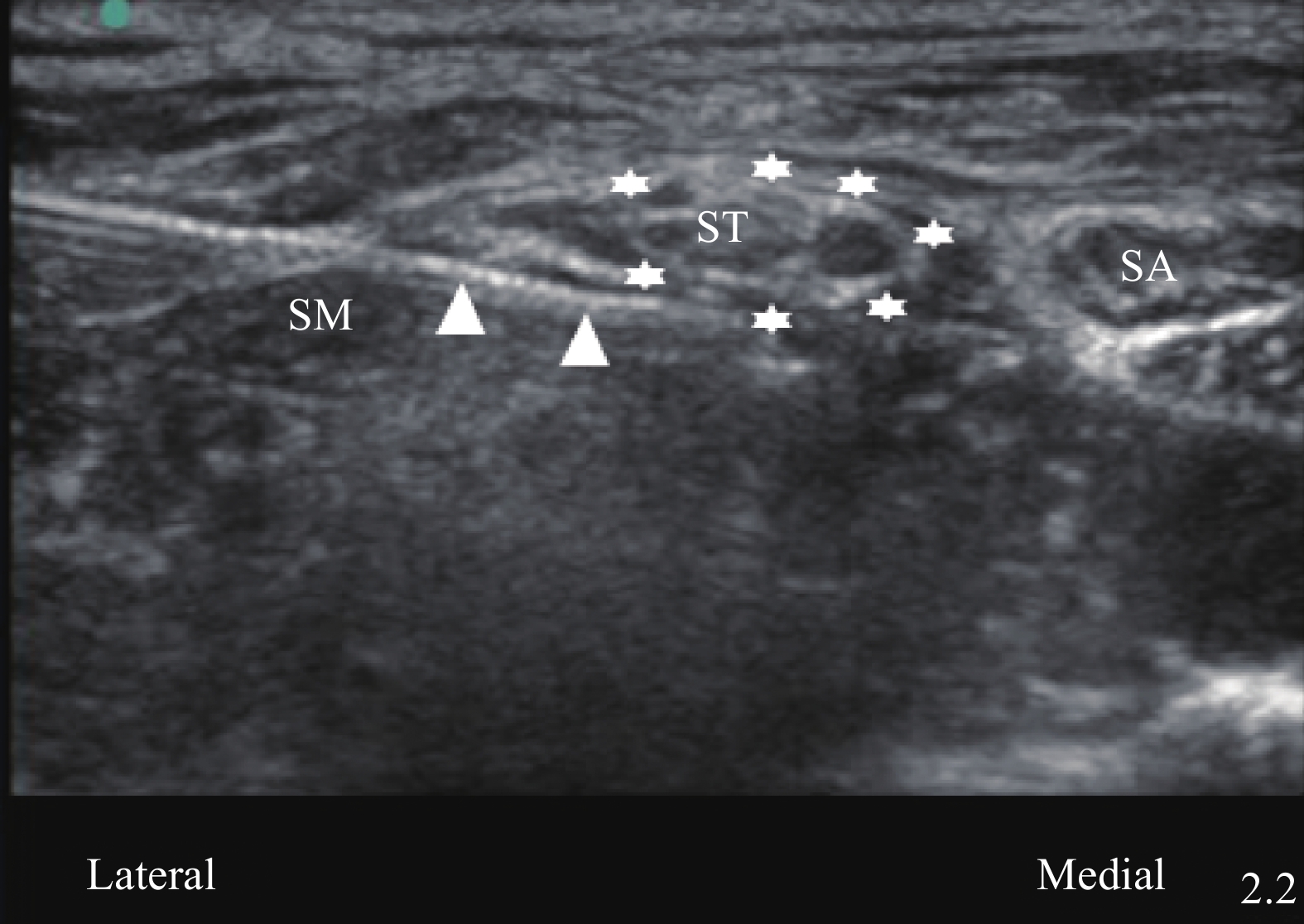
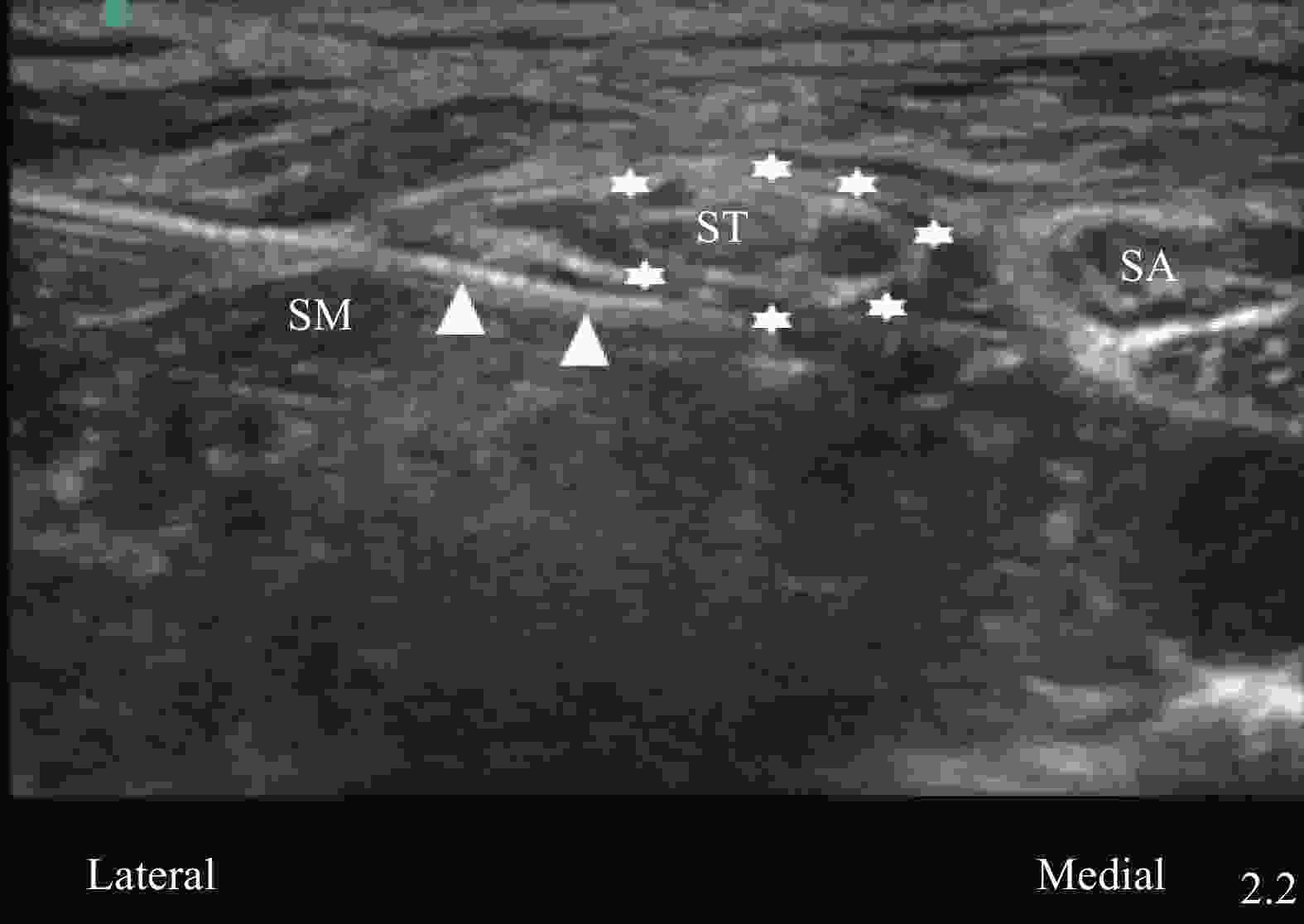
患者取平卧位,测量平静状态膈肌移动度,握力计测患侧手的握力。嘱患者头向健侧转 30°,使用高频线性探头进行定位扫查,对于ISB组,根据横突结节形状定位 C5、C6、C7 神经,找到“红绿灯征象”[7]后,平面内进针由外侧向内侧,穿过中斜角肌,采用一点法,针尖到达C5、C6外侧时回抽无血并注药,单次注射10 ml。对于ST组,在准确识别神经根的基础上探头缓慢向尾侧滑行,直至看到C5、C6汇合成臂丛上干,肩胛上神经即将分出,将该部位作为目标靶点。同样采用平面内进针,由外向内,超声引导下将针尖移至上干深面,旋转针尖使其开口朝向上干,包绕式注射5 ml 0.25% 罗哌卡因。注射完成后,将针尖移至上干浅面,阻滞针尖旋转180°,使其开口斜面继续朝向上干,包绕式注射剩余局麻药,见图1。
-
针刺拟手术区域,确认阻滞效果后,嘱患者摆侧卧位,予鼻导管吸氧及右美托咪定负荷剂量0.5~0.8 μg/kg(20 min内泵完)镇静,余以0.2~0.5 µg/(kg·h)微泵维持,直至手术结束前15 min停止泵注。
-
测量患者阻滞前以及阻滞后30 min、3 h膈肌移动度。采用低频探头(X-Porte,Sonosite),通过肝窗或脾窗测量右侧或左侧膈肌移动度。测量平静呼吸及最大深吸气时的膈肌移动幅度,测量3遍,取平均值。膈肌麻痹(HDP)的程度是通过测量膈肌移动度的减少(以百分比差值计算)来定义。完全麻痹定义平静呼吸状态,移动度减少75%~100%,部分膈肌麻痹是指平均呼吸状态移动度减少25%~75%和轻度膈肌麻痹是指下降幅度小于25%[5]。
-
患侧手全力抓持握力器,测量3次取均值。分别为阻滞前以及阻滞后30 min、3 h的平均握力。
-
采用疼痛数字评分法(NRS)评估患者疼痛程度,记录神经阻滞后0~6 h,6~12 h及12~24 h时间段内患者静息状态下NRS最高评分以及阻滞时长(从阻滞开始起,直至出现痛觉恢复的时间)。
-
记录阻滞不全、霍纳(HONOR)综合征、声嘶、术后恶心呕吐的发生情况。
-
本试验共纳入51例患者,共剔除5例。其中4例是因为ISB组阻滞效果欠佳,重新追加注射麻药,ST组1例是因对患者实施双侧臂丛上干阻滞。两组患者一般情况无统计学差异(P>0.05),见表1。
组别 例数
(例)年龄
(岁,
$\bar x $±s)性别
(例,
男/女)BMI
(kg/m2 ,
$\bar x $±s)阻滞侧
(例,
右/左)手术时间
(t/min,
$\bar x $±s)ISB组 23 58.3±10.3 11/12 24.6±2.4 13/10 81.9±8.6 ST组 23 61.1±6.6 9/14 23.8±2.5 11/12 83.7±12.5 -
ISB组患者平静呼吸状态下膈肌移动度为(2.02±0.42)cm,阻滞后30 min下降为(1.50±0.29)cm,阻滞后3 h膈肌移动度为(0.98±0.20)cm。最大深呼吸时膈肌移动度则分别为(5.30±0.70)cm、(3.53±1.04)cm和(1.86±0.58)cm。
ST组平静呼吸状态膈肌移动度为(1.91±0.21)cm,阻滞后30 min为(1.63±0.22)cm,阻滞后3 h膈肌移动度为(1.43±0.18)cm。最大深呼吸时膈肌移动度则分别为(5.17±0.48) cm、(3.51±0.95)cm和(2.29±0.55)cm。阻滞后30 min,ISB组与ST组膈肌移动度下降幅度差异无统计学意义(P>0.05),阻滞后3 h,两组之间膈肌移动度下降幅度差异显著(P<0.05)。阻滞后膈肌移动度,见表2。
时间 组别 平静呼吸 最大深呼吸 阻滞前 ISB组 2.02±0.42 5.30±0.70 ST组 1.91±0.21 5.17±0.48 阻滞后30 min ISB组 1.50±0.29 3.53±1.04 ST组 1.63±0.22 3.51±0.95 阻滞后3 h ISB组 0.98±0.20 1.86±0.58 ST组 1.43±0.18* 2.29±0.55* *P < 0.05,与ISB组比较。 根据膈肌麻痹定义,两组患者轻度麻痹、部分麻痹、完全麻痹的例数,见表3。
时间 组别 平静呼吸 轻度麻痹 部分麻痹 完全麻痹 阻滞后30 min ISB组 9(39.1) 12(52.2) 2(8.7) ST组 17(73.9) 6(26.1) 0(0.0) 阻滞后3 h ISB组 4(17.4) 15(65.2) 4(17.4) ST组 14(60.9) 9(39.1)* 0(0.0)* *P<0.05,与ISB组比较。 -
神经阻滞前,ISB组与ST组患者握力无明显差异(P=0.721),阻滞后30 min,ISB组与ST组握力下降幅度差异显著(P<0.001),阻滞后3 h,两组差异同样显著(P<0.001),ST组对握力的保留明显优于ISB组,见表4。
时间 组别 握力 P 下降幅度(%) 阻滞前 ISB组 30.94±7.64 0.721 — ST组 30.23±5.58 — 阻滞后30 min ISB组 15.20±6.15 <0.001 52.17 ST组 24.01±4.91 20.59 阻滞后3 h ISB组 6.14±2.27 <0.001 80.11 ST组 14.35±3.33 52.38 注:“—”表示未获得数据。 -
两组患者在阻滞后3~6 h,6~12 h及12~24 h 3个时间段内,NRS最高评分均具有显著差异(P<0.05),见表5。
组别 阻滞后时间段 PACU~3 h 3~6 h 6~12 h 12~24 h ISB组 0 0.57±1.16 2.74±1.25 3.39±1.27 ST组 0 0 1.74±0.86 1.83±1.07 P值 — 0.024 0.003 <0.001 注:“—”表示未获得数据。PACU表示麻醉后监护室。 -
阻滞时长是指从神经阻滞完成直至患者痛觉恢复的时间,ISB组与ST组的平均时长分别是(8.3±1.97)h和(10.9±1.26)h,存在显著差异(P<0.01)。ISB组最长阻滞时长为11.6 h,最短为4.2 h,5名患者在6 h内恢复痛觉。ST组最长阻滞时间为13.6 h,最短为8.5 h 。
-
所有入组患者均无霍纳(HONOR)综合征、声嘶、局麻药过敏及中毒的情况。
-
肩关节镜手术虽属微创手术,但术后疼痛剧烈[8]。良好的术后镇痛可以加速患者康复,从而推进ERAS进程。近些年,围绕肩关节镜手术的神经阻滞报道很多,全世界学者都努力寻找麻醉的平衡点,镇痛完全,又能有效降低膈肌麻痹的发生率[9]。
肌间沟臂丛阻滞是肩关节围术期镇痛最常用的麻醉方式。但因解剖的关系在C5、C6和(或)C7处注射局麻药常会扩散至位于前斜角肌表面的膈神经,不可避免地导致膈肌麻痹。尽管降低局麻药浓度和(或)剂量可以减少HDP的发生,但迄今为止报道用最低容量5 ml 0.75%罗哌卡因行肌间沟臂丛阻滞,HDP的发生率仍达到33%[10]。Laurent等[11]提出臂丛上干阻滞的概念,Kim也报道了采用15 ml 0.375%布比卡因行上干阻滞+监护麻醉,HDP的发生率仅为4.8%[4]。我们课题组先前报道10 ml 0.375% 罗哌卡因环形包绕上干注射,完全HDP发生率为0.0%,但部分HDP发生率仍高达87.2%。为进一步降低HDP,减少对膈肌影响,因此,本研究选择10 ml 0.25% 罗哌卡因,进一步探讨低浓度低剂量局麻药在肩关节镜围术期的临床有效性。
结果显示,采用10 ml 0.25% 罗哌卡因,阻滞后30 min,ISB组与ST组对膈肌影响无明显差异(平静时P值=0.100;最大吸气时P值=0.955),考虑可能与低浓度罗哌卡因对运动神经阻滞起效慢相关,所以较短时间内两组差异性不明显。在阻滞后3 h,两组膈肌移动度下降具有显著差异(P<0.05)。此外,本研究ISB组采用的注药方式为临床上常用的一点法,由外向内进针,穿过中斜角肌,到达C5、C6外侧时注药,10 ml 0.25% 罗哌卡因可能无法完全包绕C5、C6神经根,导致阻滞不全或镇痛时间减少。肌间沟注药部位,膈神经常可于前斜角肌表面扫查到,采用类似于臂丛上干包绕式注药方式,局麻药注射至C5内侧时,药液常直接扩散至膈神经,导致其被阻滞。尽管本研究采用迄今为止满足外科手术麻醉最低药量,但ISB组平静呼吸时完全HDP的发生率仍有17.4%,而ST组则为0.0%,主要考虑臂丛上干阻滞距离膈神经更远,膈肌麻痹发生率更低。
术后疼痛方面,ST组明显优于ISB组。Kang[5]的研究认为,臂丛上干阻滞提供与肌间沟臂丛阻滞相似的镇痛效果。但本研究发现,无论是各时间段静息痛NRS最高评分,还是阻滞时长方面,ST组均明显优于ISB组,具有显著差异,这可能归因于解剖因素与给药方式。这类手术阻滞的目的是完全阻滞C5、C6神经根(无须阻滞C5分出的肩胛背神经)。在肌间沟水平,C5、C6常位于前、中斜角肌之间,神经周围的筋膜很薄,使得C5、C6边界难以辨别,会增加神经内注射风险,而且会有部分药液扩散至C7甚至C8,导致目标神经阻滞药量减少。本研究剔除的4例阻滞不全患者,可能与上述因素有关。
在握力方面,ST组明显优于ISB组,这与先前的两项RCT结果相符[4-5]。罗哌卡因本身具有运动感觉分离的效应,浓度高低决定了运动阻滞的程度,低浓度的使用使得运动功能的保留更为显著[3]。我们课题组也尝试采用更低浓度罗哌卡因(0.15%~0.2%)或者剂量(5~10 ml)行神经阻滞,握力的保留虽然更好,但有一定比例患者阻滞不全或者达到外科麻醉需求时间过长。
综上所述,10 ml 0.25%罗哌卡因臂丛上干阻滞较肌间沟臂丛阻滞具有更长的阻滞时间,更低的HDP发生率,更优的术后镇痛效果,更好的握力保留。
Comparison of interscalene brachial plexus block and superior trunk block with ropivacaine in shoulder arthroscopic surgery
doi: 10.12206/j.issn.1006-0111.202105099
- Received Date: 2021-05-20
- Rev Recd Date: 2021-08-31
- Available Online: 2021-12-27
- Publish Date: 2021-11-25
-
Key words:
- superior trunk block /
- hemidiaphragmatic paresis /
- interscalene brachial plexus block /
- arthroscopic shoulder surgery /
- ropivacaine
Abstract:
| Citation: | ZHOU Yangyang, YAN Xiaodi, ZHANG Jinxiang, DING Peng, YANG Liye, LI Yonghua. Comparison of interscalene brachial plexus block and superior trunk block with ropivacaine in shoulder arthroscopic surgery[J]. Journal of Pharmaceutical Practice and Service, 2021, 39(6): 561-565. doi: 10.12206/j.issn.1006-0111.202105099 |






 DownLoad:
DownLoad: